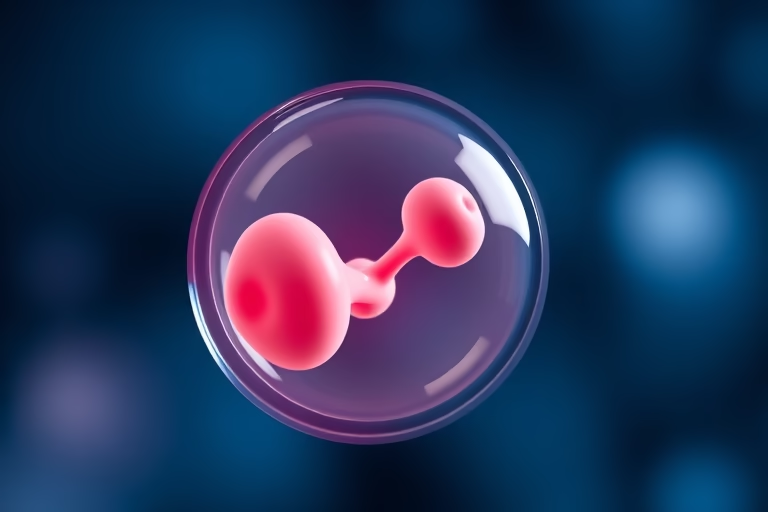
We will be talking about IVF blastocyst, a crucial aspect of in vitro fertilization (IVF). In the context of reproductive medicine, a blastocyst is an advanced stage of embryonic development that occurs about five to six days after fertilization. After fertilization, the zygote undergoes several cell divisions, forming a cluster of cells known as a morula, before developing into a blastocyst. This stage is characterized by a fluid-filled cavity, known as a blastocoel, and is divided into two different cell types: trophoblasts, which will form the placenta, and inner cell mass, which will develop into the fetus. The transition to the blastocyst stage is a critical milestone in IVF, as successful implantation into the uterine lining significantly increases the chances of pregnancy. Choosing to transfer a blastocyst instead of a cleavage-stage embryo often yields better results due to its advanced development and ability to select the healthiest embryos. This article will explore various aspects of IVF blastocysts and what potential parents should understand.
Understanding IVF Blastocyst Transfer
IVF blastocyst transfer occurs when embryos are allowed to develop for five to six days before being implanted into the uterus. This process helps researchers and healthcare professionals identify the most viable embryos based on their development stage. Transferring blastocysts, compared to earlier-stage embryos, generally leads to higher success rates in IVF due to their optimized genetic and developmental characteristics.
Embryos that develop into blastocysts have a better chance of implantation, and they may be more likely to result in a successful pregnancy. This is because blastocysts are observed to have higher developmental potential and are more fully formed than embryos at earlier stages. By transferring a single blastocyst, physicians might minimize the chances of multiple pregnancies while optimizing the chance of success.
Nevertheless, not all embryos reach the blastocyst stage. Several factors can influence embryonic development, including maternal age, egg quality, and cellular health. In some cases, only a fraction of embryos will survive to become blastocysts, leading many couples to face the emotional and financial strains of IVF.
Thus, understanding the dynamics of IVF blastocyst transfer is essential for patients undergoing fertility treatments. Effective communication with healthcare providers can set realistic expectations and help couples prepare for different outcomes.
Factors Influencing Blastocyst Formation
Numerous factors can affect the formation of blastocysts during the IVF process. Each influence can shape the success rate of embryo development. These factors include:
- Maternal Age: Women tend to have decreased egg quality as they age, which can impact embryonic development.
- Genetic Quality: Genetic abnormalities can impair embryo growth and lead to unsuccessful implantation.
- Hormonal Balance: Proper hormonal levels are critical for creating a suitable environment for embryo growth.
- Cultural Conditions: The laboratory environment, including temperature and nutrient supply, plays a significant role in blastocyst development.
Combining these factors provides a broader perspective on why some embryos may progress to the blastocyst stage while others do not. Fertility specialists often assess these elements before recommending the best treatment approach to maximize the odds of successful pregnancies.
Advantages of Blastocyst Transfer in IVF
Transferring blastocysts during the IVF process comes with several advantages. Patients and clinicians prefer this method for various reasons, including improved success rates and more efficient embryo selection.
1. Improved Implantation Rates: Studies show that blastocysts have higher implantation rates than embryos at earlier stages due to their advanced development.
2. Higher Pregnancy Rates: The chances of achieving pregnancy are considerably higher with blastocyst transfers compared to other methods.
3. Reduced Risk of Multiple Pregnancies: Transferring a single blastocyst decreases the likelihood of multiple births, which can carry various risks for both mothers and babies.
4. Increased Efficiency: Transferring embryos that are more advanced means that clinics can better select the most viable candidates, leading to careful treatment planning.
5. Psychological Benefits: Higher success rates can translate into less emotional strain on couples undergoing fertility treatments, fostering a more positive experience overall.
Disadvantages and Risks of IVF Blastocyst Transfer
While transferring blastocysts has many benefits, some disadvantages and risks need to be considered. Understanding these factors is essential for prospective parents.
1. Cost: IVF procedures, including blastocyst transfers, can be expensive and may not always be covered by insurance.
2. Emotional Toll: The IVF journey can be emotionally draining, and unsuccessful transfers can lead to additional anxiety and stress.
3. Potential for Fewer Available Embryos: Not all embryos reach the blastocyst stage, meaning fewer embryos might be available for transfer.
4. Embryo Freezing and Storage Issues: Embryos that are not used must be frozen, requiring additional storage solutions that may also incur costs.
5. Possible Health Risks: Though rare, some studies suggest that multiple pregnancies can lead to complications for both the mother and child.
How to Prepare for Blastocyst Transfer
Proper preparation for a blastocyst transfer is vital for enhancing the likelihood of success in IVF. Here are some steps to help couples adequately prepare:
- Consult Your Doctor: Engage closely with your fertility specialist to understand the process and timeline.
- Follow Pre-treatment Guidelines: Comply with any recommendations regarding medication and lifestyle changes.
- Adopt a Healthy Lifestyle: Ensure a nutritious diet, regular exercise, and stress management to improve overall health.
- Schedule Emotional Support: Participate in counseling or support groups as needed to address emotional stressors.
- Understand the Timeline: Be aware of the phases of the IVF process to streamline expectations regarding when to anticipate a transfer.
Effective preparation can elevate the chances of achieving a successful pregnancy during the IVF process, and being informed can help guide couples through potential obstacles.
Potential Success Rates of IVF Blastocyst Transfer
IVF success rates can vary significantly based on a range of factors, but understanding the average success rates associated with blastocyst transfers can provide insight to hopeful parents.
1. Maternal Age: Women under 35 typically see higher success rates, while those over 40 experience lower rates due to factors like diminished egg quality.
2. Previous History: A woman’s previous pregnancy history can play a role in predicting the chances of success in subsequent IVF cycles.
3. Health Status: Underlying health conditions or complications can also affect the individual success rate for couples undergoing IVF.
The reported success rates for blastocyst transfers range from 40% to 60% or more, depending on the above-mentioned circumstances. Consulting with fertility specialists can provide more meaningful statistics tailored to individual circumstances.
Final Thoughts
The concept of IVF blastocyst is essential in understanding in vitro fertilization processes. From its definition to the nuances of transfer, each element contributes to the larger picture of reproductive health. The advancements achieved through blastocyst transfers ultimately provide hope to couples exploring fertility options.
While there are many advantages to blastocyst transfer — including higher success rates and reduced risks of multiple pregnancies — it is necessary to consider the emotional and financial implications. Equipped with knowledge about preparation strategies and realistic expectations of success ratios, couples can foster a supportive approach in their journeys, standing a better chance of achieving their dreams of parenthood.
Ultimately, the path to parenthood may be filled with uncertainties, but understanding IVF blastocysts can empower couples and equip them with the right tools to navigate their journey effectively.
Frequently Asked Questions
1. What is a blastocyst?
A blastocyst is a stage of embryonic development that occurs approximately five to six days after fertilization. It is characterized by a fluid-filled cavity and early cell differentiation.
2. Why is it beneficial to transfer a blastocyst instead of an earlier-stage embryo?
Transferring a blastocyst generally results in higher implantation rates and pregnancy success due to its advanced development.
3. What are the risks involved in IVF blastocyst transfers?
Risks include emotional tolls, costs, the possibility of fewer viable embryos, and complications associated with multiple pregnancies.
4. How does maternal age impact the success of blastocyst transfer?
Maternal age significantly affects egg quality and can influence overall success rates, with younger women typically having higher rates.
5. What should I do to prepare for a blastocyst transfer?
Consult with your doctor, follow pre-treatment guidelines, adopt a healthy lifestyle, and manage emotional health.
Further Reading
What Type of Psychotherapy Is Best for Anxiety?