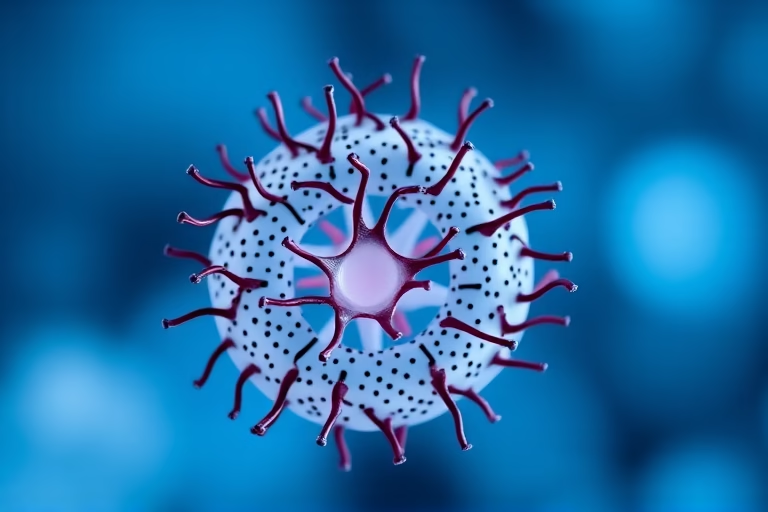
We will be talking about IVF follicles. IVF, or in vitro fertilization, is a complex process used to assist with fertility or prevent genetic problems. As part of this process, follicles play a crucial role. In a woman’s ovaries, follicles are small sacs that contain immature eggs. During the IVF process, several follicles are stimulated to grow, with the aim of retrieving mature eggs for fertilization. Understanding IVF follicles is vital for both prospective parents undergoing treatment and healthcare professionals assisting them. This article will provide a comprehensive overview of IVF follicles, including their significance in the IVF procedure, factors affecting their development, and what patients can expect during treatment.
The health of IVF follicles significantly affects the success of the IVF cycle. Follicles must be of proper size and contain healthy eggs to maximize the chances of conception. The fertility specialist will monitor follicle development using ultrasound and hormone tests to determine the best time for egg retrieval. Monitoring is critical to ensure that not too many eggs are retrieved, posing a risk of ovarian hyperstimulation syndrome (OHSS), or too few, which can reduce the chances of successful fertilization.
Understanding the Role of Follicles in IVF
Follicles are essential components in the reproductive system, particularly concerning fertility treatments like IVF. Each month, a woman produces several follicles, but typically only one becomes the dominant follicle that matures and releases an egg during ovulation. In an IVF cycle, however, medication is used to stimulate the growth of multiple follicles simultaneously. This approach enables the retrieval of several eggs, increasing the likelihood of successful fertilization and implantation.
Follicles produce hormones such as estrogen, which are vital not only for egg maturation but also for preparing the lining of the uterus for potential pregnancy. The interaction between follicles and hormones is critical for reproductive health. In an IVF cycle, the balance of hormones must be carefully monitored to optimize follicle growth and prevent complications.
Overall, understanding the function of follicles in IVF is crucial for potential parents as they navigate the challenges of infertility. By grasping how follicles affect fertility, individuals can better comprehend the IVF process and what to expect from treatment.
Factors Influencing Follicle Development
The development of follicles is influenced by various factors, both physiological and environmental. Key aspects include age, hormonal balance, genetic predisposition, and lifestyle choices. Women typically experience a decline in ovarian reserve as they age, which can impact the quantity and quality of follicles produced.
Hormonal levels play a significant role in follicular development, with Follicle Stimulating Hormone (FSH) being the primary regulator. A proper balance of hormones is necessary for stimulating the growth of follicles. Medications used during IVF treatment usually involve hormone therapy to promote optimal follicle growth.
Genetics also contribute to an individual’s response to ovarian stimulation medications. Some women may have an inherent predisposition for better follicle and egg quality, while others may struggle despite proper medical interventions.
Lifestyle choices, such as diet, exercise, smoking, and alcohol consumption, can also adversely affect follicle development. Maintaining a healthy lifestyle can improve overall fertility and enhance the outcomes of IVF treatments. Those considering IVF should consult healthcare professionals regarding their lifestyle and its impact on follicle health.
Monitoring Follicles During IVF Treatment
The monitoring of follicles during IVF treatment is a critical step to ensure a successful egg retrieval process. Fertility specialists employ ultrasound imaging and blood tests to track the development of follicles over the course of the IVF cycle.
Ultrasound allows the physician to visualize the ovaries and the growth of follicles. During this monitoring, the size and number of follicles are recorded. Typically, follicles need to be at least 18-20mm in diameter to successfully trigger ovulation or retrieval.
Alongside ultrasound, hormone levels are continually monitored through blood tests. This includes checking the levels of estradiol and progesterone, which are key indicators of follicle health and development. Abnormal hormone levels can signal issues with ovarian function and may necessitate adjustments to the treatment protocol.
All these monitoring steps are essential in determining the precise timing for egg retrieval. Proper timing helps to ensure that eggs are matured adequately without overstimulation, which can lead to complications like ovarian hyperstimulation syndrome (OHSS).
The Process of Egg Retrieval
Egg retrieval is a minor surgical procedure that forms part of the IVF treatment protocol. Once the follicles have been monitored and deemed ready, the retrieval process is initiated using a needle guided by ultrasound. This process generally occurs under sedation or anesthesia to ensure comfort.
During the procedure, the physician uses a thin needle to collect the eggs from the mature follicles individually. This process typically takes about 20-30 minutes, and recovery from sedation is quick. After retrieval, the eggs are examined for quality, and those that are mature are selected for fertilization.
The success of retrieving healthy eggs largely depends on the quality of the follicles and their proper management throughout the IVF cycle. Good communication with healthcare professionals before and after egg retrieval is crucial, allowing individuals to address any questions or concerns they may have.
Potential Complications Associated with Follicle Development
While follicle development is integral to the IVF process, it can also present several complications. One pertinent concern is Ovarian Hyperstimulation Syndrome (OHSS), which can occur when the ovaries react excessively to the hormone injections used to stimulate follicle growth.
Symptoms of OHSS can range from mild discomfort and bloating to severe abdominal pain and fluid accumulation in the abdomen. In severe cases, hospitalization may be necessary. Monitoring hormone levels and follicle development closely can help mitigate risks associated with OHSS.
Other potential complications may include poor egg quality, leading to unsuccessful fertilization or embryo development. This highlights the importance of addressing lifestyle factors and other influences on follicle health prior to and during treatment.
Education and awareness regarding potential complications can empower individuals and couples going through IVF, allowing them to work closely with healthcare teams to navigate challenges effectively.
The Impact of IVF Follicles on Success Rates
The quality and quantity of IVF follicles have a substantial impact on overall success rates in fertility treatments. Numerous research studies have shown that women with a higher number of mature eggs tend to have better outcomes concerning pregnancy rates.
A multitude of factors, including age, hormonal levels, and lifestyle choices, plays a significant role in determining the capability of follicles to yield viable eggs. Younger women typically have a greater ovarian reserve, translating into better chances of harvesting healthy eggs.
While having a higher number of follicles is beneficial, egg quality also cannot be overlooked. Quality influences the embryo’s viability after fertilization, affecting implantation and overall success. Comprehensive evaluations carried out during the IVF process can help ascertain each patient’s unique profile, guiding tailored treatment approaches for optimal results.
Can Follice Health Be Improved for IVF?
Several strategies may improve follicle health in preparation for IVF treatment. Nutritional considerations and dietary adjustments can influence follicle development positively. Consuming a balanced diet rich in vitamins, minerals, and antioxidants can support overall hormone regulation and reproductive health.
Stress management is also key to improving reproductive health. Engaging in regular physical exercise, practicing mindfulness, and obtaining adequate rest can help reduce stress levels, promoting better hormonal balance.
Additionally, avoiding harmful substances like tobacco and excessive alcohol can enhance follicle health. Screenings and consultations with fertility specialists can provide tailored recommendations that address individual health issues and lifestyle factors, contributing to healthier follicles and improved fertility outcomes.
Final Thoughts
In summary, understanding IVF follicles is essential for those considering fertility treatments. Follicles play a critical role in the reproductive process, and their health can directly influence the success of IVF cycles. Knowing the factors affecting follicle development, the monitoring procedures involved, and managing risks are paramount steps in achieving successful outcomes. Individuals should consider their lifestyle and available medical interventions to enhance follicle health and overall chances of conception.
As potential parents embark on their fertility journey, knowledge and communication with healthcare professionals will empower them to address obstacles effectively. By understanding the complexities surrounding IVF follicles, individuals can transform their reproductive health, moving towards achieving their dreams of parenthood.
Frequently Asked Questions
Further Reading
What Type of Psychotherapy Is Best for Anxiety?