When considering the process of in vitro fertilization (IVF), understanding the number of embryos implanted is crucial for prospective parents. The journey can be complex, with many factors influencing the decision on how many embryos to transfer during a single IVF cycle. This blog will explore the details surrounding this topic, answering the fundamental question: how many embryos are implanted during IVF? We will define IVF and its significance, and delve into related aspects to provide a comprehensive understanding.
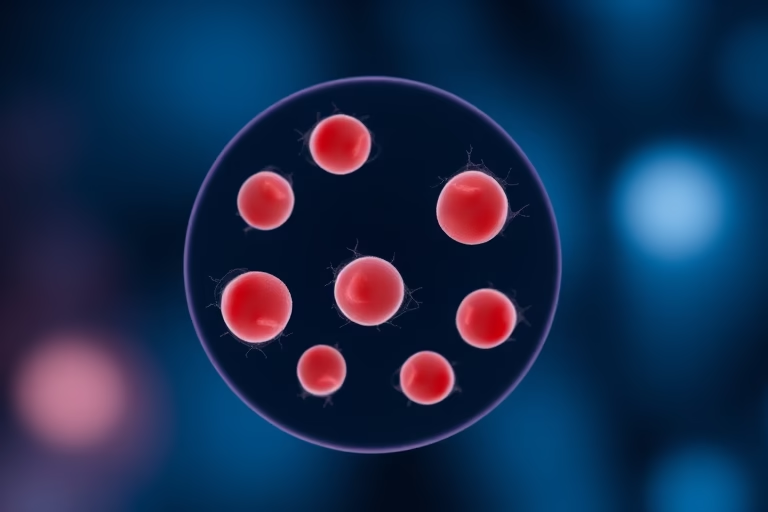
In vitro fertilization is a fertility treatment that involves the extraction of eggs and the capturing of sperm outside the body, creating embryos in a lab setting. Once embryos are developed, they can be implanted into a woman’s uterus. The number of embryos transferred during the process is influenced by several factors, including the age of the woman, the quality of the embryos, and previous reproductive history. Understanding these elements helps optimize the chances of successful implantation and pregnancy, while also considering the potential risks of multiple pregnancies.
The Purpose of Transferring Embryos
The decision regarding how many embryos to implant during IVF is based on enhancing the likelihood of a successful pregnancy. The aim is for at least one embryo to successfully implant and develop into a healthy fetus. It is vital to balance this goal with the risks associated with multiple pregnancies and the emotional and physical toll they can take on parents.
Typically, clinics take multiple factors into consideration:
- Patient’s age
- Quality of embryos
- History of previous IVF attempts
- Utter health conditions
This tailored approach allows medical professionals to make informed recommendations about how many embryos will be implanted, ensuring the best possible outcome for the couple.
Multiple Embryo Transfers: Benefits and Risks
The prospect of transferring multiple embryos can increase the chance of a successful pregnancy. The benefits include a higher success rate overall as there are more than one potential embryo that can implant and grow. For women who are older or who have had unsuccessful IVF cycles in the past, this approach may be particularly beneficial.
However, risks accompany transferring multiple embryos. The likelihood of a multiple pregnancy—twins, triplets, etc.—increases significantly. Multiple pregnancies can carry greater health risks for both the mother and babies, such as preterm labor, gestational diabetes, and complications in prenatal care. Therefore, thorough counseling and consideration of personal circumstances is essential before deciding on the number of embryos to implant.
Factors Affecting the Number of Embryos Transferred
Several factors can affect the decision on how many embryos to transfer during IVF treatment. It is essential to tailor the approach to maximize the chances of pregnancy while minimizing risks.
Key factors include:
- Age of the female patient: Younger patients frequently transfer fewer embryos due to their higher chances of success with single transfers.
- Quality of embryos: The quality and developmental stage of embryos play a significant role. High-quality embryos might yield higher implantation success rates, thus favoring single transfers.
- Previous IVF history: Previous unsuccessful cycles may lead to the decision of transferring multiple embryos in subsequent attempts to improve chances.
- Health history: Underlying health conditions may necessitate a change in the number of embryos implanted.
In summary, the decision is not solely a clinical one. It embodies ethical considerations and personal wishes, making it intricate and individualized.
Single Embryo Transfer: A Growing Trend
In recent years, a trend toward single embryo transfer (SET) has gained traction in IVF practices. SET is based on the idea of minimizing the risks associated with multiple pregnancies while still maintaining successful outcomes. The advancement of embryo selection techniques means that clinics can increasingly identify and select the highest quality embryos for transfer, thus improving the odds of success with fewer embryos.
Many studies indicate that the overall success rates for single embryo transfer are comparable to multiple transfers, especially when using preimplantation genetic testing (PGT). This trend also promotes a healthier pregnancy atmosphere, allowing for more controlled monitoring of the pregnancy and reducing complications associated with multiple births.
Emotional and Financial Considerations
The emotional and financial burden of IVF treatment cannot be overstated. Couples undergoing IVF face significant stress and anxiety, which can be exacerbated by failed attempts. The number of embryos implanted can weigh heavily on decision-making.
The cost of IVF cycles is also a significant consideration. Transferring multiple embryos may seem advantageous in terms of increased success chances, but additional cycles may still be necessary. Couples must consider their financial situation and support systems when weighing how many embryos to transfer.
Best Practices and Recommendations from Professionals
Healthcare professionals continue to research and refine best practices in embryo transfer protocols. Current recommendations generally advocate for a cautious approach:
- Consider patient-specific factors before deciding on the number of embryos.
- Utilize single embryo transfer when appropriate, especially for younger women with high-quality embryos.
- Discuss with patients the possible risks and benefits of multiple embryos, ensuring informed consent.
- Regularly monitor advancements in embryo selection technologies and adjust practices accordingly.
Staying updated with current practices helps to optimize the IVF process, making it a more successful and fulfilling experience for parents.
Final Thoughts
Understanding how many embryos are implanted during IVF is an essential part of the journey for couples seeking to conceive. It is not a one-size-fits-all answer; medical history, age, and embryo quality all play integral roles in the decision-making process. Ensuring the right approach maximizes the chances of successful implantation while also considering the associated risks.
As we see more clinics adopt practices like single embryo transfer, the IVF landscape continues to evolve, emphasizing safety and health for both mothers and their potential children. Open conversations with healthcare providers about the optimal number of embryos to transfer allow couples to make informed decisions tailored to their unique circumstances.
Frequently Asked Questions
- What is IVF? In vitro fertilization (IVF) is a fertilization process where an egg and sperm are combined outside the body, creating embryos that can be implanted in the uterus.
- How many embryos are usually implanted during IVF? Depending on individual circumstances, typically between one to three embryos are implanted during a single IVF cycle.
- What factors influence the number of embryos transferred? Factors include the patient’s age, embryo quality, previous reproductive history, and overall health.
- What are the risks of transferring multiple embryos? Transferring multiple embryos increases the chances of multiple pregnancies, which carries higher health risks for both the mother and babies.
- Is single embryo transfer safe? Yes, studies show that single embryo transfers can be just as effective as multiple embryos, particularly when using high-quality embryos.
Further Reading
What Type of Psychotherapy Is Best for Anxiety?