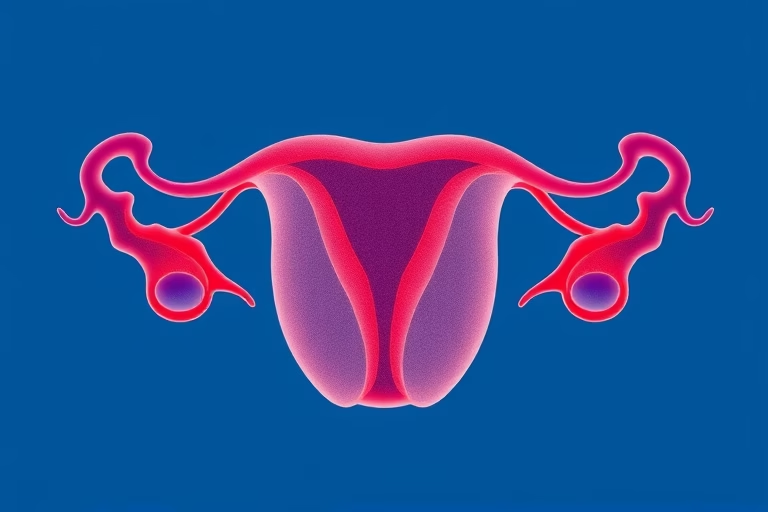
We will be talking about endometrial thickness for IVF. Endometrial thickness plays a crucial role in the success of in vitro fertilization. The endometrium is the inner lining of the uterus, which thickens and prepares itself for a potential pregnancy during the menstrual cycle. For successful implantation of an embryo, optimal endometrial thickness is essential. In women undergoing IVF, the right thickness can significantly affect their chances of conceiving. Studies suggest that a thickness between 7mm and 14mm is considered ideal for embryo implantation. Different factors can influence this thickness, including hormonal levels, body weight, and age. Understanding these aspects can help potential parents enhance their chances of having a child through IVF.
Understanding Endometrial Thickness
Endometrial thickness refers to the measurement of the uterine lining, which is vital for pregnancy. During the menstrual cycle, the endometrium undergoes changes due to hormonal fluctuations. At the beginning of the cycle, the endometrium is thin, typically about 2-4mm. As estrogen levels rise, the lining thickens in preparation for implantation of a fertilized egg. Ideally, by the time of ovulation, the thickness should reach between 7mm and 14mm to support a viable pregnancy.
During IVF procedures, doctors monitor endometrial thickness closely using ultrasound. A thick enough lining increases the chances of embryo implantation. However, if the endometrium is too thin, it may not provide a suitable environment for the embryo to attach and grow. Hormonal treatments are often used during IVF cycles to ensure optimal endometrial development. Understanding this process empowers women undergoing IVF to make informed decisions about their treatment and improve their outcomes.
Factors Influencing Endometrial Thickness
Multiple factors can influence the thickness of the endometrium. These factors include hormonal levels, lifestyle choices, medical conditions, and age.
Hormonal Levels: Hormones, particularly estrogen and progesterone, play a pivotal role in the regulation of endometrial thickness. During the follicular phase, rising estrogen levels stimulate the growth of the lining. After ovulation, progesterone helps stabilize and maintain it. Abnormal levels of these hormones can lead to an inadequate endometrial lining.
Body Weight: A woman’s body weight can significantly impact her reproductive health. Women who are underweight may have lower estrogen levels, which can result in a thinner endometrial lining. Conversely, obesity can lead to hormonal imbalances that also affect endometrial thickness.
Medical Conditions: Certain medical conditions, such as polycystic ovary syndrome (PCOS) or endometriosis, can disrupt hormonal balance or uterine structure, impacting endometrial thickness. These conditions may require specific management to optimize the chances of IVF success.
Age: Age is a significant factor in women’s reproductive health. As women age, hormonal changes can occur, leading to variations in cycle regularity and endocrine function. Older women may experience thinner endometrial lining, which can affect fertility.
The Role of Hormones in Endometrial Preparation
Hormones play a crucial role in preparing the endometrium for implantation during the menstrual cycle. In a typical cycle, follicle-stimulating hormone (FSH) stimulates the ovaries to produce follicles that contain eggs. These follicles secrete estrogen, which promotes the growth of the endometrium.
As estrogen levels rise, the endometrium thickens and becomes enriched with blood vessels and nutrients to create a hospitable environment for a fertilized egg. When ovulation occurs, luteinizing hormone (LH) surges, leading to the release of an egg from the ovaries. Subsequently, the ruptured follicle transforms into the corpus luteum, which produces progesterone.
Progesterone is vital for maintaining the thickness of the endometrium. It stabilizes the lining and further prepares it for implantation. If an embryo implants successfully, it will trigger the production of human chorionic gonadotropin (hCG), supporting the pregnancy. If no implantation occurs, hormone levels drop, leading to menstruation.
For women undergoing IVF, hormonal medications are often used to stimulate the ovaries and regulate these hormone levels, enhancing the endometrial lining for a favorable implantation environment.
Strategies to Optimize Endometrial Thickness
Women undergoing IVF can take several measures to optimize their endometrial thickness, increasing their chances of successful implantation. Here are some strategies:
- Diet: Consuming a balanced diet rich in vitamins and minerals can support hormonal health. Foods high in omega-3 fatty acids, antioxidants, and whole grains are particularly beneficial.
- Hydration: Staying well-hydrated supports overall health and can improve blood flow to the uterus, promoting a healthy endometrial lining.
- Regular Exercise: Engaging in moderate physical activity helps maintain a healthy body weight and hormonal balance.
- Stress Management: High stress levels can negatively impact hormonal balance. Practices such as yoga, meditation, or deep-breathing exercises can be helpful.
- Medication: Discussing hormone replacement therapy options with a healthcare provider can also be beneficial in achieving optimal endometrial development.
Consulting with a fertility specialist will allow women to tailor their strategies based on their unique situations, enhancing their chances of achieving pregnancy through IVF.
Monitoring Endometrial Thickness during IVF
Monitoring endometrial thickness is a standard practice during IVF treatment. Healthcare providers typically use transvaginal ultrasound to measure the endometrial lining regularly. This monitoring helps assess whether the endometrium is growing adequately in response to hormonal medications.
During this monitoring phase, physicians will look for specific measurements. An endometrial thickness greater than 7mm is generally considered adequate, while thickness approaching 10-14mm is often ideal for successful implantation. If the endometrium is found to be insufficiently thick, adjustments may be made to the treatment plan, such as increasing hormone dosages or altering the timing of embryo transfer.
Endometrial monitoring not only aids in optimizing the conditions for implantation but can also provide insights into women’s overall reproductive health. Regular assessments enable timely decisions and can improve the success rates of IVF procedures.
Embryo Transfer Timing and Endometrial Thickness
The timing of embryo transfer is a critical factor in successful IVF outcomes, closely linked to endometrial thickness. The transfer typically occurs when the endometrium is at its optimal thickness, indicating that it is ready to receive the embryo. This timing aligns with the current reproductive cycle of the patient and aims for synchronized development of both the embryo and the endometrium.
Embryo transfer can take place during a natural cycle or a medicated cycle, depending on individual circumstances. In natural cycles, practitioners closely monitor ovulation, ensuring the transfer aligns with the optimal period for implantation. In medicated cycles, hormonal medications facilitate synchronized development of the endometrium, allowing for precise transfer timing.
Ultimately, careful timing improves the chances of successful implantation, making it essential for fertility specialists to consider not just the endometrial thickness but also the timing in the reproductive cycle.
Potential Risks of Abnormal Endometrial Thickness
Abnormal endometrial thickness can pose risks to conception and healthy pregnancy. An excessively thick endometrium can indicate hormones imbalances or conditions like endometrial hyperplasia, which may lead to complications. Patients with abnormal thickness often require further evaluation, which may include hormonal assessments or imaging tests to determine underlying issues.
If the endometrium is too thin, the risks include challenges with embryo implantation. An inadequate lining does not facilitate the necessary environment for an embryo to thrive and grow. This situation may lead to unsuccessful IVF attempts and necessitate further medical advice.
Women should consult healthcare providers about the implications of abnormal endometrial thickness, alongside potential treatment options, emphasizing the need for early intervention and monitoring.
Final Thoughts
Endometrial thickness is a fundamental aspect of IVF, influencing the likelihood of embryo implantation and overall success rates. Understanding the precise nature of this relationship can empower women undergoing fertility treatments. Factors such as hormonal levels, body weight, lifestyle choices, and age play major roles in determining endometrial thickness. Through appropriate strategies, patients can enhance their chances of successful implantation.
Monitoring endometrial thickness is essential in IVF protocols, providing valuable insights for adjusting treatment plans to optimize outcomes. The timing of embryo transfer is equally vital, entailing synchronization between embryo development and the endometrial phase. By comprehensively recognizing and addressing the factors impacting endometrial thickness, women can work more effectively with their healthcare providers to achieve their IVF goals.
In summary, endometrial thickness for IVF is not just a clinical measurement; it represents significant dynamics around reproductive health and fertility. Taking proactive steps, from lifestyle adjustments to medical interventions, can support heightened success during the IVF journey.
Frequently Asked Questions
- What is the ideal thickness of the endometrium for IVF?
The optimal range is generally 7mm to 14mm for the best chances of embryo implantation. - How is endometrial thickness measured?
Endometrial thickness is typically measured using a transvaginal ultrasound. - Can endometrial thickness be increased?
Yes, through hormonal treatments, lifestyle changes, and proper diet, women can enhance endometrial thickness. - What happens if the endometrium is too thin?
A thin endometrium can decrease the chances of successful embryo implantation in IVF. - How often is endometrial thickness monitored during IVF?
Monitoring frequency varies, but it’s generally assessed multiple times before embryo transfer to ensure appropriate thickness.
Further Reading
What Type of Psychotherapy Is Best for Anxiety?