We will be talking about hysteroscopy before IVF. Hysteroscopy is a medical procedure that allows doctors to examine the inside of the uterus using a thin, lighted tube called a hysteroscope. This procedure can be useful for diagnosing or treating issues within the uterus, including abnormalities like fibroids, polyps, or uterine anomalies. Its significance becomes pronounced when preparing for an In Vitro Fertilization (IVF) procedure, as a clear assessment of the uterine environment can greatly impact the success of embryo implantation. By ensuring that the uterus is healthy and free of any obstructions, hysteroscopy plays a critical role in increasing the chances of a successful IVF outcome. Understanding this procedure is essential for individuals or couples seeking fertility treatments.
What is Hysteroscopy?
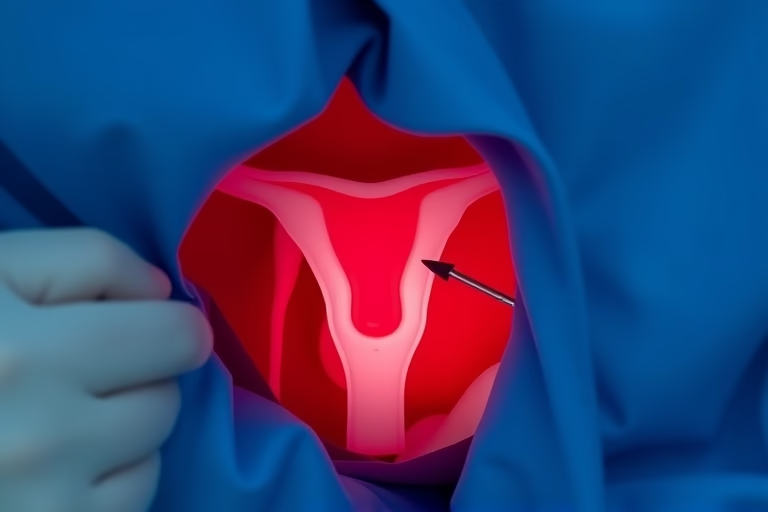
Hysteroscopy is a minimally invasive surgical procedure used to inspect the interior of the uterus. The hysteroscope is inserted through the vagina and cervix into the uterus, allowing doctors to view the uterine lining directly. This examination can be performed for various reasons, including diagnosing conditions like endometrial polyps or fibroids, investigating abnormal bleeding, or assessing infertility. In the context of IVF, it provides valuable insights into the uterine condition and helps in planning the most effective treatment course. Hysteroscopy can also facilitate the removal of problematic growths or tissue, thus optimizing conditions for implantation.
This procedure can either be performed in an office setting for diagnostic purposes or in a hospital under general anesthesia for surgical interventions. Patients are usually advised on what to expect, and the recovery time is typically short, making it a relatively convenient choice for many seeking advanced reproductive care.
Importance of Hysteroscopy Before IVF
The significance of hysteroscopy before initiating an IVF procedure cannot be understated. Not only does it provide critical information about the female reproductive system, but it also enables medical professionals to address any uterine abnormalities that may hinder implantation. Many fertility specialists recommend hysteroscopy as a preparatory step in the IVF process.
By identifying and treating any issues, such as polyps or fibroids, hysteroscopy can create a more favorable environment for embryo attachment. Moreover, this procedure can uncover inflammatory conditions or anatomical anomalies that may not be detected through other imaging methods, such as ultrasounds.
As IVF involves careful monitoring and timing, ensuring optimal uterine health simplifies the process for both patients and medical practitioners. Overall, it enhances the likelihood of a successful pregnancy, making hysteroscopy before all IVF procedures a standard recommendation in fertility treatments.
How Hysteroscopy is Performed
The procedure for hysteroscopy involves several steps. Initially, the patient undergoes a preparatory assessment, which may include blood tests and imaging studies. On the day of the procedure, the patient may be given medication to help relax or anesthetize.
Next, the physician gently inserts the hysteroscope through the cervix into the uterus. A saline solution is usually infused to distend the uterine cavity, providing a clearer view. The doctor then examines the uterine lining via the hysteroscope, which is equipped with a camera and light.
If any abnormalities are found, additional instruments may be introduced through the hysteroscope for biopsy or surgical removal, such as the extraction of polyps or fibroids. The duration of the procedure is typically under an hour, and once completed, patients will spend some time in recovery before they are discharged.
Post-procedure instructions generally include avoiding strenuous activities, sexual intercourse, and the use of tampons for a short period to ensure proper healing. Overall, hysteroscopy is a safe procedure with minimal risks, making it a preferred choice for uterine evaluations.
Potential Risks of Hysteroscopy
While hysteroscopy is considered a low-risk procedure, it is essential to be aware of potential complications. Some of the risks associated include:
Patients should discuss any concerns with their doctor prior to undergoing hysteroscopy. In most cases, the benefits of obtaining clear insight into uterine health significantly outweigh the risks involved in the procedure.
Preparation for Hysteroscopy
Effective preparation for hysteroscopy involves both emotional and physical components. Understanding the procedure and what to expect can help ease anxiety. Patients should follow the guidance provided by their healthcare provider, which typically includes:
- Scheduling the procedure during a specific phase of the menstrual cycle, often right after menstruation ends.
- Avoiding sexual intercourse, douching, or using tampons for about 2 days prior to the procedure to minimize contamination.
- Discussing current medications or health conditions with their physician to ensure safety.
- Arranging for transportation, as patients may feel groggy if sedation is used.
By preparing adequately for hysteroscopy, patients can enhance their comfort and cooperation during the procedure, contributing positively to the overall experience.
Recovery After Hysteroscopy
Recovery after hysteroscopy is generally quick, but patients should adhere to certain guidelines for a smooth recovery period. Immediately after the procedure, some mild cramping or spotting may occur, which is typical.
To facilitate healing, patients are usually advised to:
- Rest and refrain from engaging in strenuous activities or exercise for a day or two.
- Avoid sexual intercourse until cleared by the healthcare provider.
- Monitor any unusual changes such as heavy bleeding or signs of infection, and contact the doctor if these occur.
- Use over-the-counter pain relievers as directed to manage any discomfort.
Most women are able to return to normal activities within a few days but should participate in follow-up appointments to ensure everything is healing correctly. Staying informed and responsive to one’s body will support a healthy recovery process.
Planning for IVF After Hysteroscopy
After undergoing hysteroscopy, many women feel encouraged to proceed with IVF planning. Once clear from any abnormalities and having a healthy uterine environment, patients can approach IVF with increased confidence. Fertility specialists often tailor strategies based on the findings of the hysteroscopy.
This may involve scheduling IVF cycles, monitoring hormone levels, and discussing embryo transfer protocols. The odds of successful implantation are often maximized following hysteroscopy. Many couples report feeling a sense of relief after addressing uterine health, which can translate into a more positive pregnancy journey.
Collaborating with a qualified fertility specialist ensures that patients receive the best possible outcomes from both hysteroscopy and IVF.
Final Thoughts
Hysteroscopy before IVF is an essential aspect of reproductive health. This procedure allows for a comprehensive evaluation of the uterine environment, enabling the identification and treatment of any factors that could impair the chances of successful implantation. Understanding the intricacies of hysteroscopy, from its importance to the potential risks and recovery, empowers patients to make informed choices about their fertility journey.
Preparing adequately for hysteroscopy, ensuring open communication with healthcare providers, and following recovery guidelines fosters a supportive and successful environment for pursuing IVF. With the right knowledge and careful planning, couples facing fertility challenges can enhance their chances of achieving a successful pregnancy. Hysteroscopy serves as a proactive step toward enhancing reproductive health and maximizing the effectiveness of IVF treatments.
As the world advances in fertility technology, trusting the process and maintaining a hopeful outlook can significantly impact the outcomes of these carefully orchestrated efforts.
Frequently Asked Questions
1. What are the benefits of hysteroscopy before IVF?
Hysteroscopy offers the chance to detect and treat uterine abnormalities that may affect IVF success. By ensuring a healthy uterine environment, it increases the likelihood of successful implantation.
2. Is hysteroscopy a painful procedure?
Patients may experience mild discomfort or cramping during the procedure. Local or general anesthesia is often utilized to minimize pain, and recovery is usually quick.
3. How long does recovery take after hysteroscopy?
Most patients can return to normal activities within a few days. However, it is advisable to avoid strenuous activities and sexual intercourse for a designated recovery period.
4. How soon can I start IVF after hysteroscopy?
Generally, couples can proceed with IVF shortly after hysteroscopy, once cleared by their healthcare provider. Each case is unique, and timing will be based on individual health assessments.
5. Are there any risks involved with hysteroscopy?
As with any medical procedure, there are potential risks such as infection, uterine perforation, and excessive bleeding. Discussing concerns with the healthcare provider can ensure appropriate precautions are taken.
Further Reading
What Type of Psychotherapy Is Best for Anxiety?