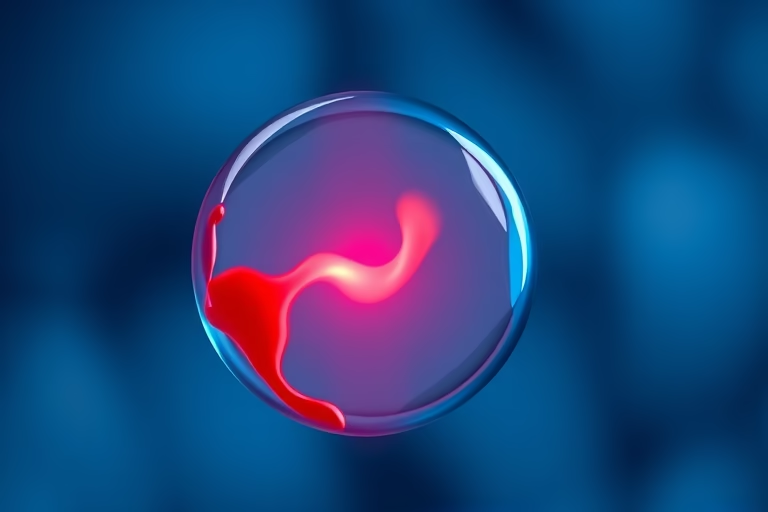
Understanding Implantation Failure Bleeding
Implantation failure bleeding refers to the light spotting or bleeding that occurs when a fertilized egg fails to implant successfully in the lining of the uterus. This phenomenon can happen during the early stages of pregnancy as the body adjusts to changes following conception. While it is normal for some women to experience this type of bleeding as part of their menstrual cycle, women trying to conceive may see it as a sign of implantation failure. The experience can provoke emotional distress and uncertainty, especially when evaluating the chances of a successful pregnancy. It is critical to differentiate between normal menstrual bleeding, implantation bleeding, and the possible signs of complications. Understanding the context, causes, and implications of implantation failure bleeding is essential for women who are seeking to understand their reproductive health.
Common Symptoms Associated with Implantation Failure Bleeding
Women commonly experience different symptoms when dealing with implantation failure bleeding. Although there may be some commonalities, it is important to remember that each woman’s experience is unique. Typical symptoms include:
- Light spotting or bleeding, which is often lighter than a regular period
- Cramping or abdominal discomfort
- Changes in breast tenderness or sensitivity
- Nausea or mood swings
- General signs of hormonal shifts
In most cases, these symptoms do not necessarily indicate a problem, but if a woman experiences intense pain or heavy bleeding, it is advisable to consult a healthcare provider. Recognizing these symptoms and how they relate to one’s cycle can provide valuable insights into reproductive health.
How Implantation Failure May Occur
Implantation failure can happen due to various factors that may affect the endometrium or the embryo itself. The endometrium must be in an optimal state to support implantation. Factors that can lead to failure include hormonal imbalances, inadequate endometrial lining, or chromosomal abnormalities in the embryo. When the lining is either too thin or too thick, it does not adequately nourish a developing embryo. Furthermore, if the embryo has any genetic issues, it might not develop properly, leading to failure during implantation.
Another aspect to consider is the timing of implantation. The embryo must implant at a specific time for proper hormonal signaling and nutrient transfer. A late implantation can also lead to failure as the uterine environment may no longer be supportive. Stress, lifestyle factors, and pre-existing health conditions can also interfere with implantation.
Role of Hormones in Implantation Failure
Hormones play a crucial role in the processes surrounding conception, implantation, and overall reproductive health. The menstrual cycle is regulated by hormones, including estrogen and progesterone, which prepare the endometrium for implantation. If hormone levels are inconsistent, the preparation may be compromised, leading to difficulties in implantation.
Progesterone is particularly important during the luteal phase of the menstrual cycle. It helps thicken the uterine lining and makes it more receptive to a fertilized egg. If hormone levels drop prematurely, the lining may shed before a fertilized egg has a chance to implant successfully.
Woman’s health conditions, such as polycystic ovary syndrome (PCOS) or hormonal disorders, can contribute to hormonal imbalances, further complicating successful implantation. Hormonal assessments and potential corrective measures may be necessary for those experiencing repeated implantation failures.
Diagnosing Implantation Failure
To diagnose implantation failure bleeding and its underlying causes, healthcare providers may utilize a combination of methods:
- Medical History: Reviewing a patient’s medical history to look for any patterns or issues related to their menstrual cycle and past pregnancies is essential.
- Physical Examination: A thorough examination can include pelvic assessments to evaluate uterine health.
- Hormonal Assessments: Blood tests measured for hormone levels, especially progesterone, can help determine hormonal balance.
- Imaging: Sometimes, ultrasound technology may be used to look for any abnormalities in the uterus.
The process of diagnosing implantation failure demands a multidisciplinary approach and should include consultation with fertility specialists, especially for women who have experienced recurrent pregnancy loss or prolonged difficulties in conceiving.
Coping Mechanisms and Emotional Support
Facing implantation failure is emotionally taxing. Women may experience feelings of sadness, frustration, or disappointment. It is vital to acknowledge these feelings and seek emotional support. Some effective coping mechanisms include:
- Reaching out to support groups or communities with similar experiences.
- Consulting mental health professionals who specialize in fertility issues.
- Practicing mindfulness or stress-relief techniques.
- Keeping a journal to express emotions and thoughts.
Building a solid support system—whether among family, friends, or healthcare providers—can significantly enhance emotional well-being. Counseling can provide coping strategies and valuable resources for managing emotions during this challenging time.
When to Consult a Doctor Regarding Implantation Failure Bleeding
In some cases, implantation failure bleeding may not require immediate medical attention. However, there are instances when consulting a doctor becomes necessary. Women should seek medical guidance under the following circumstances:
- Experiencing heavy bleeding similar to a menstrual flow
- Severe abdominal cramps or pain
- Bleeding persisting for more than a few days
- Having a history of miscarriages or reproductive health issues
- Signs of infection, such as fever or unusual discharge
Receiving expert medical advice can provide clarity, and interventions may be needed to explore fertility options or address underlying health issues.
Final Thoughts
Implantation failure bleeding can be a source of confusion and distress for many women. Understanding what it is, why it occurs, and its associated symptoms play a crucial role in deciphering one’s reproductive health. Hormonal balance, proper uterine preparation, and timing are key aspects of successful implantation. Detecting implantation failure requires medical scrutiny that includes detailed assessments and emotional support strategies. Consulting a healthcare provider can guide women through their options for future attempts to conceive as well as emotional resources for coping with the challenges of implantation failure.
The journey of conceiving can be complex, and not every experience aligns with expectations. It is vital to acknowledge that bleeding during this early stage may happen but does not always imply failure. Women are encouraged to document any symptoms they experience and communicate openly. Remember, seeking professional help is a pivotal step in navigating this journey.
Frequently Asked Questions
1. What is the difference between normal menstruation and implantation bleeding?
Implantation bleeding is usually lighter in color and flow compared to typical menstrual bleeding. It also occurs around the time a woman would expect her period but is often accompanied by fewer symptoms.
2. Can lifestyle factors contribute to implantation failure?
Yes, factors such as stress, smoking, excessive alcohol consumption, and poor diet can adversely affect hormonal balance and uterine health, possibly leading to implantation failure.
3. Is implantation failure common?
It is estimated that implantation failure occurs in a significant number of conceptions, particularly among women with certain health conditions or those undergoing fertility treatments.
4. Do I need to see a doctor if I suspect implantation failure bleeding?
If you experience heavy bleeding, severe pain, or have a history of reproductive issues, seeking medical advice is highly recommended for proper evaluation and care.
5. Can implantation failure bleeding recur with multiple pregnancies?
Yes, recurrent implantation failure can occur in women with previous pregnancy loss. Consulting with a fertility specialist may provide insights into potential issues.
Further Reading
What Type of Psychotherapy Is Best for Anxiety?