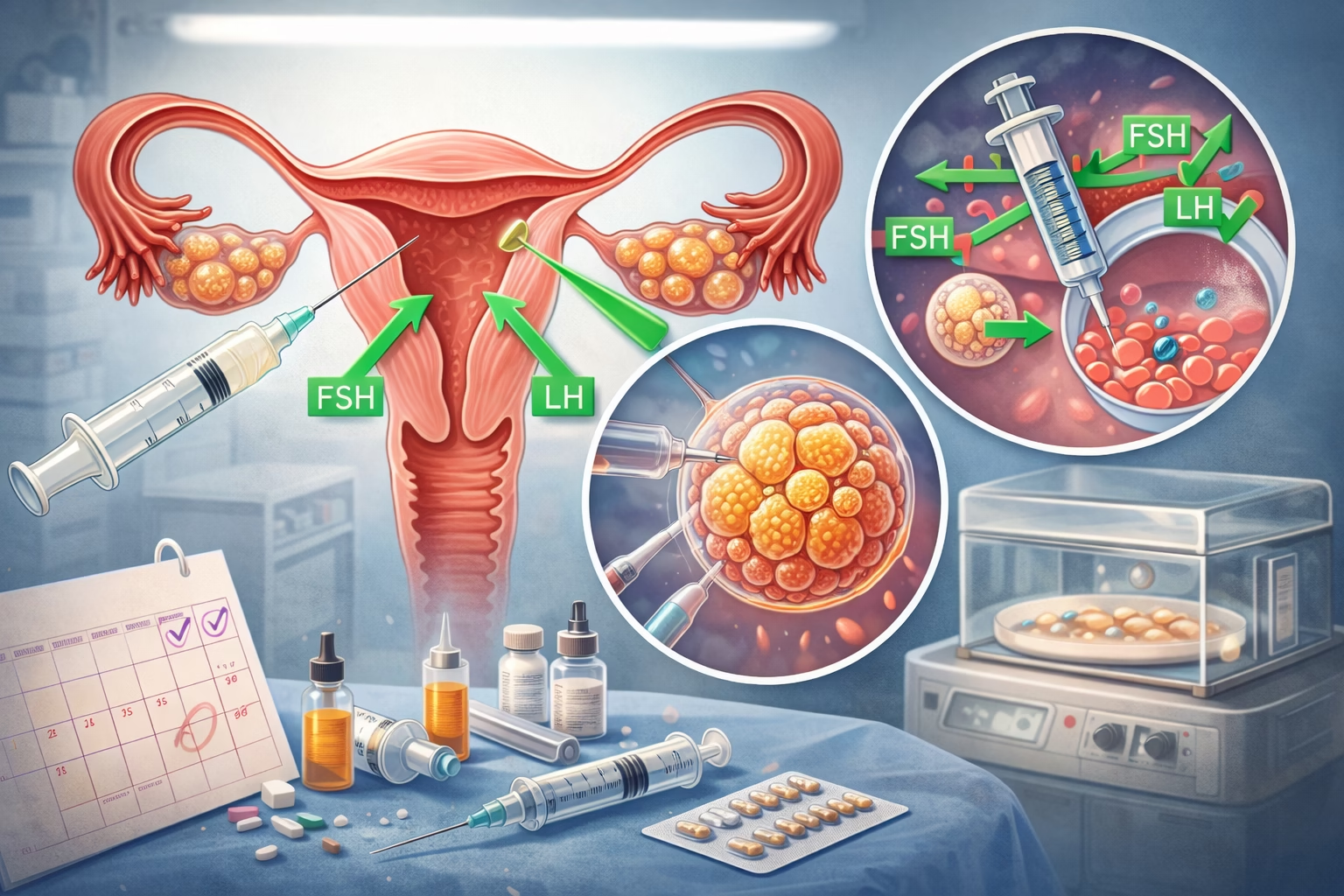
We will be talking about the IVF immune protocol, an essential aspect for couples undergoing assisted reproductive technologies like in vitro fertilization (IVF). This protocol addresses the immune factors that may affect IVF success. Many women face infertility challenges due to immune system disorders that can adversely influence conception and pregnancy. The IVF immune protocol is tailored to assess and manage these immune responses, aiming to create a favorable environment for embryo implantation and development.
Understanding the IVF immune protocol involves delving into how the immune system interacts with reproduction. The body’s immune system protects against foreign invaders, yet during conception, a balance must be struck to allow the embryo to grow without being rejected. Treatments under the IVF immune protocol may include therapies to modulate the immune response, making this protocol critical for those facing unexplained infertility or recurrent pregnancy loss.
What Is Immunology in Reproductive Health?
Immunology studies the immune system’s role in health and disease, and its application in reproductive health has gained importance. In reproduction, the immune system’s role is complex. While it protects the body from infections, it must also recognize and tolerate the embryo, which is partly foreign due to genetic material from both parents. If the immune system reacts adversely, it can lead to complications such as implantation failure or miscarriage.
Understanding the synergy between immunology and reproductive health is essential. Research indicates that conditions like autoimmune diseases, where the immune system mistakenly attacks the body’s tissues, can hinder fertility. Addressing these conditions can pave the way for successful pregnancies.
Autoimmune Disorders and IVF
Autoimmune disorders can significantly impact fertility, making it crucial to investigate this aspect when couples are struggling to conceive. These conditions lead to the production of autoantibodies that target the body’s cells, including reproductive organs. Common disorders include lupus, rheumatoid arthritis, and thyroiditis.
For women with such disorders, the IVF immune protocol often includes testing for specific autoantibodies and inflammatory markers. Treatment may involve immunosuppressive therapies, which could potentially enhance the chances of successful embryo implantation. Addressing these underlying issues is vital, as untreated autoimmune conditions can lead to pregnancy complications.
Natural Killer Cells and Infertility
Natural killer (NK) cells play a dual role in reproductive health. While essential for defending against infections and controlling tumor growth, an overactive response can undermine fertility. High levels of NK cells in the uterus are associated with implantation failure and miscarriage.
In the context of the IVF immune protocol, testing for elevated NK cell activity can provide insights into potential fertility issues. Treatments may include immunomodulatory therapies designed to balance NK cell activity, improving the chances of conception and a successful pregnancy.
The Role of Cytokines in Fertility
Cytokines are signaling molecules that mediate immune responses, and they play a pivotal role in reproduction. Imbalances in cytokine levels can lead to inflammatory responses that adversely affect embryo implantation. Certain cytokines promote implantation and pregnancy maintenance, while others may lead to rejection.
The IVF immune protocol often assesses cytokine levels in women experiencing infertility. By addressing these imbalances, healthcare professionals can create a more conducive environment for successful implantation, thereby enhancing fertility outcomes.
Testing for Immune Factors in IVF
To implement an effective IVF immune protocol, a comprehensive assessment of immune factors is essential. Testing may include evaluating autoimmune markers, NK cell activity, and cytokine levels. These tests help identify specific immune-related issues hindering fertility.
Understanding a patient’s immune profile allows healthcare providers to tailor treatments effectively. Personalized protocols can lead to better outcomes for those struggling with infertility, ensuring that all potential adverse immune responses are managed appropriately.
Therapeutic Approaches in the IVF Immune Protocol
There are various therapeutic approaches under the IVF immune protocol to enhance the likelihood of successful implantation and pregnancy. Treatments may include immunotherapy, such as intravenous immunoglobulin (IVIG), which helps modulate the immune response and reduce inflammation.
Additionally, corticosteroids may be used to suppress abnormal immune reactions that could impede embryo implantation. These therapies aim to create a more favorable uterine environment by addressing specific immune system issues identified through testing.
Lifestyle Modifications to Support IVF Success
While medical interventions are crucial, lifestyle modifications also play a significant role in enhancing fertility outcomes. Maintaining a balanced diet rich in antioxidants, managing stress levels, and engaging in regular physical activity can improve overall health and help optimize the immune system.
Additionally, women are encouraged to avoid smoking and excessive alcohol consumption, as these factors can adversely affect reproductive health. Integrating holistic practices such as yoga and meditation can further support emotional well-being during the IVF process.
Emotional Support and Counseling During IVF
Undergoing IVF can be emotionally taxing, making emotional support and counseling an important aspect of the IVF immune protocol. Understanding the emotional toll infertility can take is essential for both partners. Seeking support from counselors or support groups can help manage stress and anxiety associated with the process.
Emotional health plays a crucial role in overall well-being and reproductive health. Couples are encouraged to communicate openly with each other and to seek professional help if feelings of despair or isolation arise. This holistic approach to addressing both physical and emotional health can significantly enhance the IVF journey.
Final Thoughts
The IVF immune protocol represents a comprehensive approach to addressing fertility challenges grounded in immune factors. Understanding how the immune system impacts reproductive health is vital for couples facing unexplained infertility or recurrent pregnancy loss.
Through targeted testing and personalized treatment plans, healthcare professionals can effectively manage immune-related issues that may hinder successful conception and pregnancy maintenance. Interventions may include addressing autoimmune disorders, regulating NK cell activity, balancing cytokine levels, and providing necessary therapies to optimize the uterine environment.
Moreover, lifestyle modifications and emotional health play critical roles in improving fertility outcomes. A balanced diet, stress management, and supportive counseling enhance the overall experience for couples navigating the IVF process.
By taking a holistic approach through the IVF immune protocol, individuals can empower themselves on their journey to parenthood, creating a more favorable foundation for conception and pregnancy. Success in IVF often arises from a combination of medical treatments and a supportive environment conducive to both physical and emotional well-being.
Frequently Asked Questions
Further Reading
What Type of Psychotherapy Is Best for Anxiety?