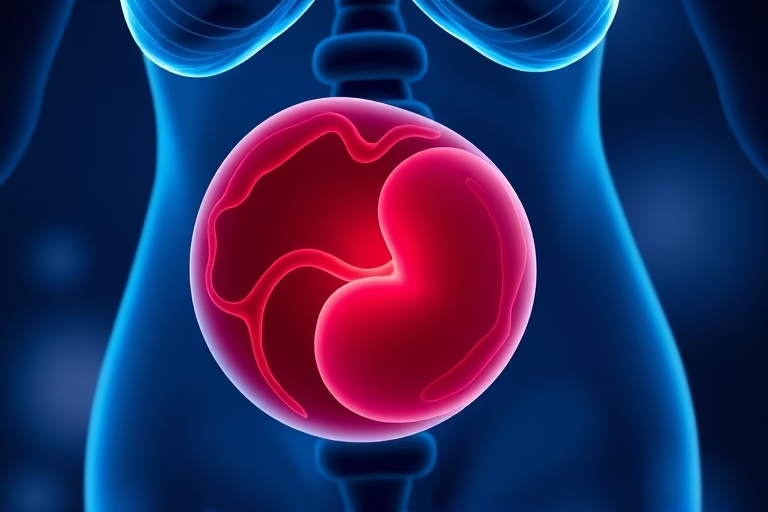
We will be talking about why does IVF cause subchorionic hemorrhage. In vitro fertilization (IVF) is a commonly used assisted reproductive technology that helps many couples conceive. During the IVF process, embryos are transferred to the uterus, and in some cases, it can lead to a condition called subchorionic hemorrhage. This refers to bleeding that occurs between the chorion, which is the outer membrane surrounding the embryo, and the uterine wall. Understanding the relationship between IVF and subchorionic hemorrhage is essential for both medical professionals and couples undergoing fertility treatments. This article explores the causes and implications of subchorionic hemorrhage in the context of IVF, providing insights and guidance for those affected by this condition.
Understanding Subchorionic Hemorrhage
Subchorionic hemorrhage is a type of bleeding that can occur during early pregnancy, particularly after embryo implantation. It results from the accumulation of blood between the chorionic membrane and the uterus. While it can happen in any pregnancy, its prevalence appears to be heightened in pregnancies resulting from IVF. The reasons for this increased incidence can vary, but it is crucial to understand that subchorionic hemorrhage does not always indicate a negative outcome for the pregnancy. Many women with this condition go on to have healthy pregnancies.
Identifying subchorionic hemorrhage typically involves ultrasound imaging during routine check-ups. This condition can lead to various symptoms, including spotting or bleeding, but some women may remain asymptomatic. Although subchorionic hemorrhage raises concerns about potential complications, many medical professionals view it with cautious optimism since most cases resolve without adverse effects on pregnancy. Understanding this condition is vital for women undergoing IVF treatments, as their awareness can aid in early detection and management.
Connection Between IVF and Subchorionic Hemorrhage
The connection between IVF and subchorionic hemorrhage involves several factors, including the method of embryo transfer, hormonal treatments, and the number of embryos implanted. IVF procedures often involve hormonal stimulation to encourage multiple egg production, which can lead to increased vascularity or fragile blood vessels in the uterus. These changes may predispose women to subchorionic hemorrhage after embryo transfer.
Additionally, the technique used for embryo transfer, and the use of non-invasive procedures can also impact the likelihood of developing subchorionic hemorrhage. In some cases, the manipulation during the procedure can cause disruption to the uterine lining, leading to bleeding. Understanding this connection is critical for both clinicians and patients as it allows for better risk assessment and management.
Risk Factors for Subchorionic Hemorrhage in IVF Pregnancies
The presence of subchorionic hemorrhage is influenced by various risk factors, especially in pregnancies conceived via IVF. Some of these risk factors include:
- Age: Women over 35 are at a higher risk.
- Multiple embryos: Transferring more than one embryo increases the likelihood of bleeding.
- Uterine abnormalities: Pre-existing conditions such as fibroids can elevate risks.
- Previous history: Women who have experienced hemorrhage in previous pregnancies may be more prone to subchorionic hemorrhage.
Identifying these risk factors is essential for healthcare providers to prepare and inform patients regarding the possibility of subchorionic hemorrhage and the necessary monitoring protocols to follow.
Diagnosis and Monitoring of Subchorionic Hemorrhage
Diagnosis of subchorionic hemorrhage is typically done through ultrasound imaging. Healthcare providers may perform a transvaginal ultrasound to visualize the uterus and detect the presence of blood clots around the gestational sac. Monitoring strategies can vary, but they usually include regular appointments to assess the status of the hemorrhage and monitor fetal development.
Women diagnosed with subchorionic hemorrhage should remain vigilant and report any new or worsening symptoms. Healthcare professionals may recommend reduced physical activity or other precautions to minimize the risk of complications. Close monitoring remains a key preventive measure, and ultrasound examinations will provide timely insights into the condition’s progression.
Potential Complications of Subchorionic Hemorrhage
While many cases of subchorionic hemorrhage resolve without complications, there are potential risks associated with this condition. The severity and outcomes can vary, but potential complications include:
- Miscarriage: Severe hemorrhage can increase the risk of losing the pregnancy.
- Preterm labor: In some cases, subchorionic hemorrhage can lead to contractions and early delivery.
- Placental abruption: A more serious condition where the placenta detaches from the uterus prematurely.
- Intrauterine growth restriction: Bleeding may affect fetal growth due to insufficient blood flow.
It is essential to communicate openly with healthcare providers about any concerns regarding these potential complications to ensure appropriate monitoring and interventions.
Management Options for Subchorionic Hemorrhage
Management of subchorionic hemorrhage primarily focuses on monitoring and managing symptoms. Routine follow-up appointments are crucial for assessing the size and impact of the hemorrhage. In most cases, women are advised to rest and avoid activities that could exacerbate bleeding.
If significant bleeding occurs or signs of complications arise, additional interventions may be warranted. Potential options include:
- Medications: The use of progesterone may help support pregnancy and reduce the risk of miscarriage.
- Cervical cerclage: In cases where the cervix may be weak, stitches can help support the pregnancy.
- Close monitoring: Regular ultrasounds to monitor fetal health and the progression of the hemorrhage.
Women undergoing IVF should remain closely connected with their healthcare team to actively participate in their management plan and address any changing symptoms swiftly.
Prevention Strategies for Subchorionic Hemorrhage
While not all cases of subchorionic hemorrhage can be prevented, certain strategies can reduce risk factors associated with this condition during IVF. These strategies include:
- Healthy lifestyle: Maintaining a balanced diet, regular exercise, and avoiding substances like tobacco and alcohol can improve overall reproductive health.
- Regular medical check-ups: Monitoring underlying health conditions and adhering to fertility protocols as advised by healthcare professionals.
- Limit physical strain: Reducing activities that place pressure on the body during early pregnancy can help minimize risks.
By addressing these factors, couples can create a healthier environment for conception and increase their chances of a successful pregnancy.
Final Thoughts
The issue of why does IVF cause subchorionic hemorrhage is one of significant importance for individuals and couples navigating the complexities of assisted reproductive technology. While subchorionic hemorrhage can be concerning, it is essential to understand that not every instance results in complications. Knowledge of the condition can empower individuals undergoing IVF to make informed decisions and better engage in discussions with their healthcare providers. Pre-emptively identifying risk factors, understanding diagnosis and monitoring protocols, and adopting management strategies are crucial to managing subchorionic hemorrhage effectively. By creating an open dialogue about these topics and focusing on healthy practices, patients and their providers can work together to enhance pregnancy outcomes.
Frequently Asked Questions
- What are the signs of subchorionic hemorrhage?
Signs can include light bleeding or spotting, but some women may be asymptomatic. Ultrasound imaging is necessary for a proper diagnosis.
- Is subchorionic hemorrhage dangerous?
While it can lead to complications, many cases resolve on their own, and many women go on to have healthy pregnancies.
- How is subchorionic hemorrhage detected?
Diagnosis is usually made through ultrasound, which helps visualize any bleeding around the gestational sac.
- Can subchorionic hemorrhage affect fetal development?
In some instances, it may impact fetal growth, but many pregnancies progress normally despite the hemorrhage.
- What should I do if I experience bleeding during IVF treatment?
Contact your healthcare provider immediately for an evaluation and guidance on the next steps.
Further Reading
What Type of Psychotherapy Is Best for Anxiety?